Medical need and indication
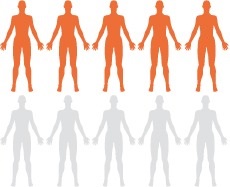
Up to 50 % of all term pregnant women are planned for start of labor with conventional treatments, which carries a high risk of complications for both mothers and infants.
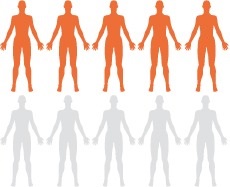
Up to 50 % of all term pregnant women are planned for start of labor with conventional treatments, which carries a high risk of complications for both mothers and infants.